Cholecystolithiasis
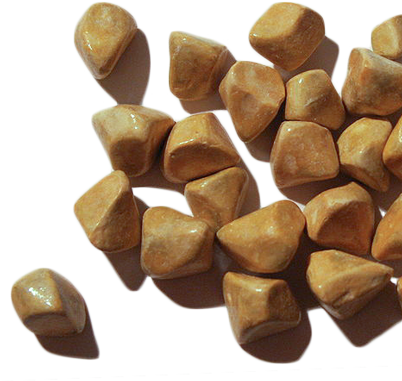
Gallstones are a common disorder due in part to the Western diet. Gallstones are not in themselves pathological, but the complications they may cause. In ca. 75% of cases, gallstones remain asymptomatic and are often only found incidentally during routine sonography.
Gallstones are especially common in overweight women around 40 years old who have given birth and are fair skinned (female, fat, forty, fertile, fair). This is however only a broad generalization and does not of course mean that patients without these traits are not liable to gallstones.
Symptoms & Diagnosis
Symptomatic cholecystolithiasis can cause right side upper abdominal pain and colic. These symptoms are nonspecific and require clarification, including gastroscopy, to rule out a gastric or duodenal ulcer.
Fever, elevated inflammatory values, and a positive Murphy’s sign are indicative of an acute cholecystitis. In ultrasound, a typical thickening of the wall is seen, and triple layering of the gall bladder. This phenomenon is of course an artefact, the gall bladder wall always exhibits multiple layers and not only when it is inflamed. Ultrasound devices, however,
do not have sufficient resolution to always show this. Only if there is edema of the gallbladder wall secondary to inflammation are the layers far enough apart to show this phenomenon. In laboratory diagnostics particular value is placed on cholestasis parameters like bilirubin, transaminases and especially alkaline phosphatase. Elevated cholestasis values point to the presence of bile duct stones. These usually lodge at the narrowest point just before the papilla of Vater and the junction of the bile duct and duodenum. This is an area, however, that is difficult to view on ultrasound due to the superposition of intestinal gas in the duodenum. An indirect sign of extrahepatic cholestasis
is the dilation of the common bile duct. If this exceeds 6-9 mm, an ERC should be performed prior to any surgery. In this procedure, which uses a special side-view endoscope, the papilla of Vater is dilated and the bile duct stone removed through this papillotomy. This procedure is an excellent alternative to intraoperative bile duct revision, which may however become necessary if a stone cannot be removed endoscopically. Bile duct stones can trigger a pancreatitis, which is termed a biliary pancreatitis.
MURPHY’S SIGN
If the patient catches his or her breath while reporting pain when the gallbladder meets the examiner’s hand, this is a positive Murphy’s sign and an indication of an acute cholecystitis.
COURVOISIER‘S SIGN
The combination of painless jaundice and an enlarged gallbladder is termed Courvoisier’s sign. If a hard gallbladder is palpated in a patient with jaundice without causing pain, the Courvoisier’s sign is positive, indicating a pancreatic head carcinoma until proved otherwise.
Chronic pancreatitis can also impede drainage of bile, leading to an obstructive jaundice. This, however, is usually associated with pain.
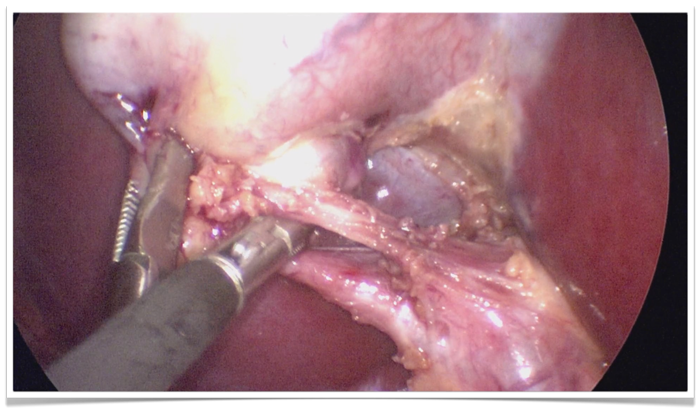
Endoscopic retrograde cholangiopancreatography (ERCP) of a hydropic gallbladder with stones. Dormia basket in a widely dilated hepatic duct.
Endoscopic Retrograde Cholangiography & Papillotomy
ERC has the drawback that the papillotomy can trigger a pancreatitis. In up to 1‰ (←?) of patients, this follows a fulminant necrotizing course with high morbidity and lethality. This underscores the gravity of the examination. Ultrasound can only suggest a bile duct stone is present but not show it directly. Before incurring the risk associated with ERC, therefore, a magnetic resonance cholangiopancreatography (MRCP), i.e. imaging of the bile ducts using MRT, can be performed to confirm or exclude the presence of a bile duct stone.
If a bile duct stone is found, ERC is indicated, if not, not. A further advantage of MRCP is that the surrounding tissue is also imaged, which can aid in the differential diagnosis of a cholestasis.
Indications for Surgery
Indications for cholecystectomy are demonstration of gallstones or biliary sludge with corresponding symptoms. The gallbladder is not removed because it has a stone, but because it can form stones
Acute cholecystitis is of course an indication for surgery. What remains to be determined is when to perform the surgery. While symptomatic cholecystolithiasis is an indication for elective surgery, acute cholecystitis surgery should be performed immediately or during the inflammation-free interval following antibiotic therapy. The longer the inflammation lasts, the more the gall bladder adheres to the adjacent jejunum or duodenum, meaning surgery should occur earlier rather than later or, if appropriate, after a few weeks if the clinical presentation allows it.
The operation today is performed as a minimally invasive procedure in which the gallbladder is removed though an access in the navel. This single-port technique requires an experienced laparoscopic surgeon, since the room for maneuver is even less than that of conventional laparoscopy using four trocars.
The operation can also be performed through the body’s natural openings, such as the stomach or vagina. With regard of surgical technique, however, the interventions differ not only in their views of the OP area. Open access is also possible, which is classically performed through a right side costal margin incision. This access is available, for example, for a perforated gallbladder or if the patient’s overall condition would not tolerate a laparoscopy.
Cholecystectomy
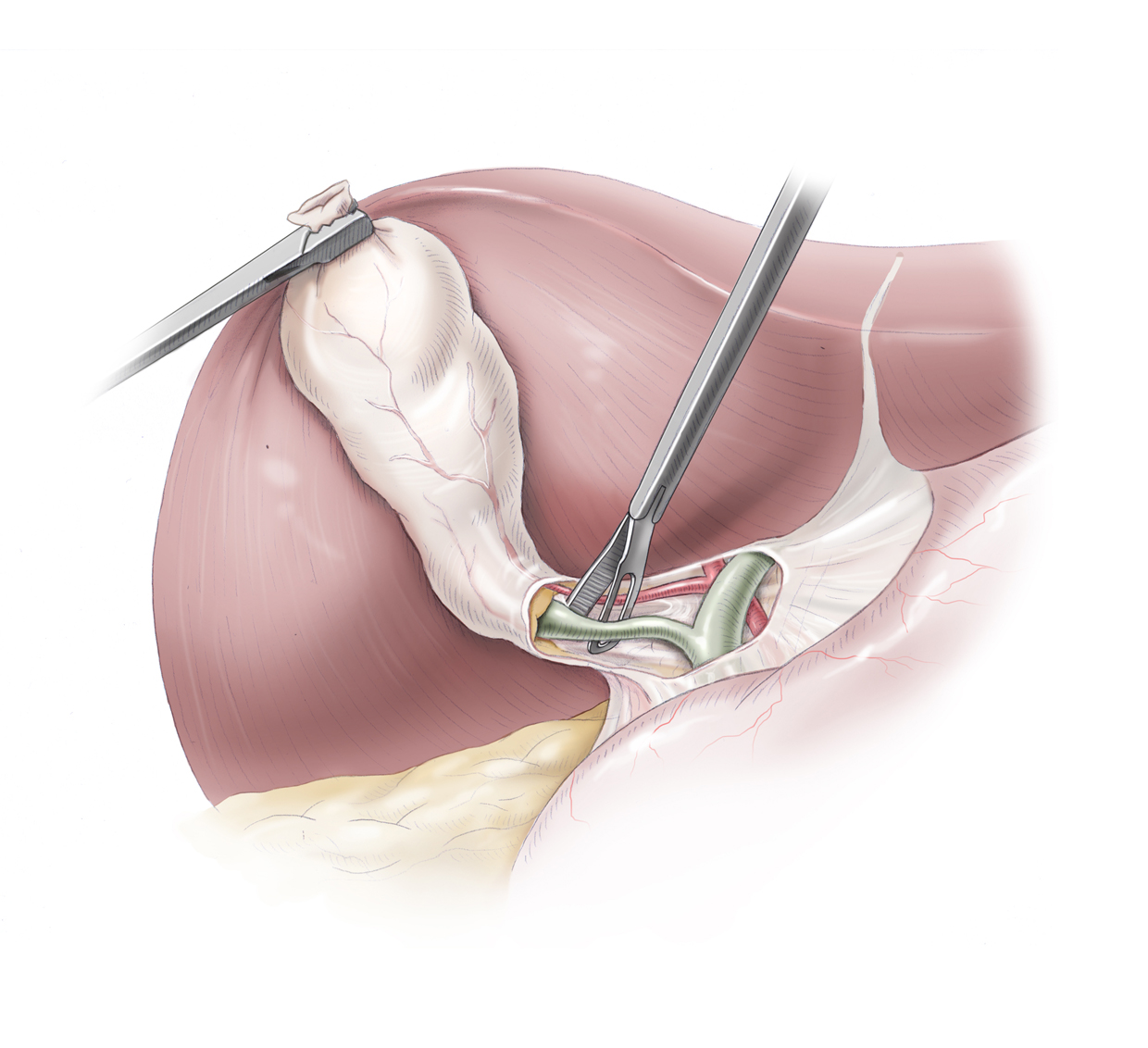
The landmarks of the operation are exposure (Darstellung) of Calot's triangle and identification of the cystic artery and cystic duct.
Calot's triangle is comprised of the cystic duct, the hepatic duct, and the inferior border of the liver. It marks the site where the structures leading to the gallbladder are to be dissected.
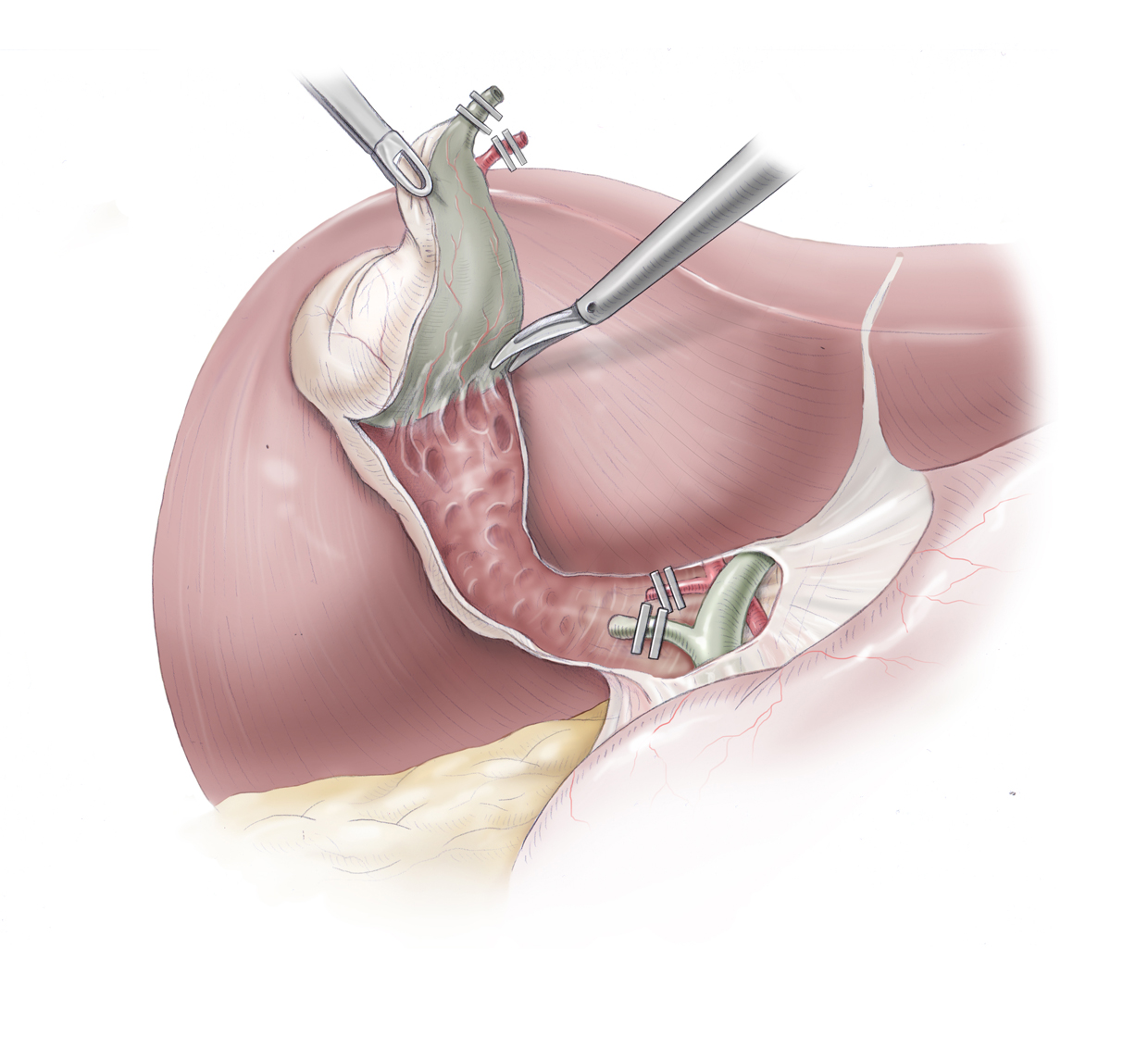
Before these structures are clipped with titanium clips and severed, they must be definitively identified. Under no circumstances may the ductus choledochus be clipped or an hepatic artery with an atypical course be severed.
Once this step has been completed, the gallbladder is dissected from bottom to top out of the gallbladder bed of the liver. It is important to always dissect in the correct layer so as not to injure the gallbladder or cut into the liver.
At conclusion of the procedure the gallbladder is packed in a plastic specimen pouch and removed from the body. A drain remains only if the gallbladder was severely inflamed, or if there was intraoperative leakage of bile. If stones fall out of the gallbladder they must all be found and retrieved.
OP site, cystic duct and cystic artery
Single-Port Cholecystectomy
Single-Port Cholecystectomy
A further advance in minimally invasive surgery is reduced-port or single-port surgery, where the number of trocars needed for laparoscopy is reduced, leaving still fewer visible scars.
The surgical principle differs only with regard to the number of instruments used, the OP steps are the same as in the conventional laparoscopic method, which is generally performed through 4 trocars.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia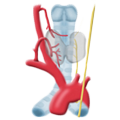 Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma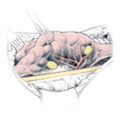 Hyperparathyroidism
Hyperparathyroidism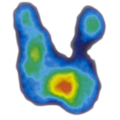 Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia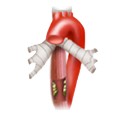 Esophageal Carcinoma
Esophageal Carcinoma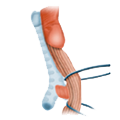 Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD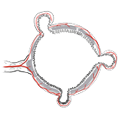 Divertikulitis
Divertikulitis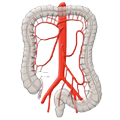 Colon Carcinoma
Colon Carcinoma Proktology
Proktology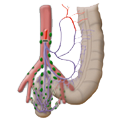 Rectal Carcinoma
Rectal Carcinoma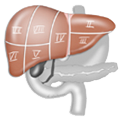 Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions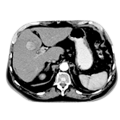 Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis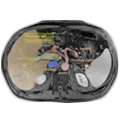 Pancreatic carcinoma
Pancreatic carcinoma